Feb 12, 2024 | Chiropractic, Dr. Annette Ghelfi
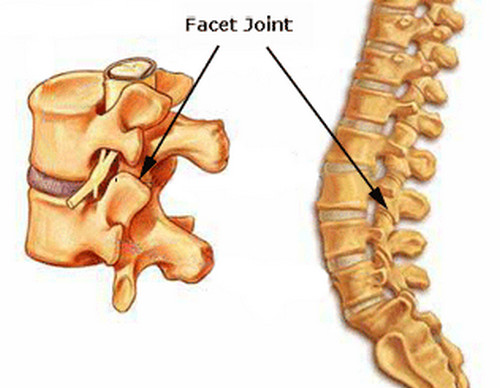
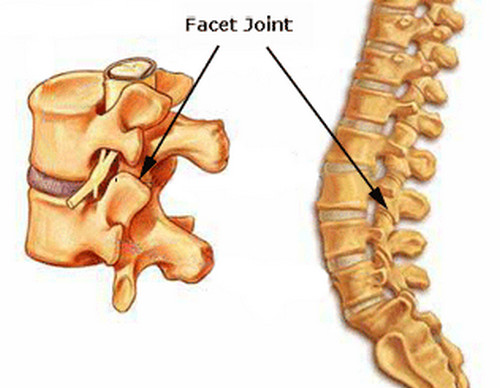
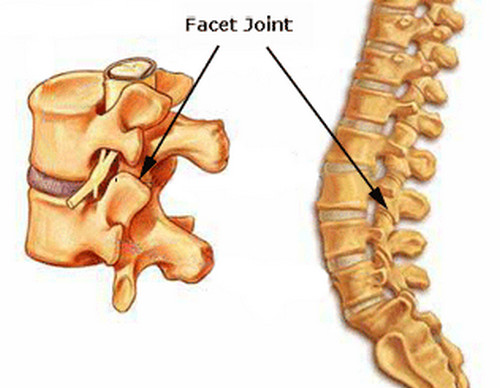
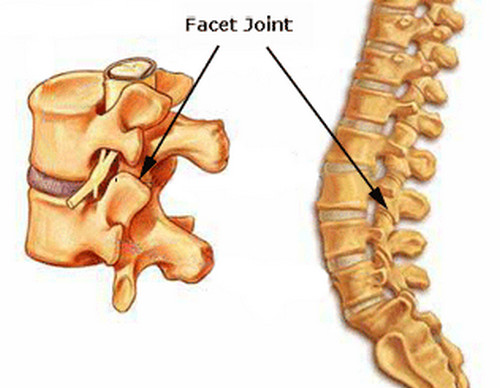
If you are a patient at Performance Health Center, you have probably heard your doctors use the term facet syndrome to describe the cause of your pain syndrome. But what is facet syndrome? Have you ever been physically active over the weekend then the next day...
Nov 7, 2023 | Chiropractic, Did you know, Dr. Tom Ball, Health, Performance Health Center
That is the Jeopardy answer to this question: What causes sudden onset of pain in joints with sometimes severe swelling, with no know injury to these joints. This “disease” mimics Gout, but is not Gout as there are no uric acid crystals involved, instead a...
Jun 4, 2019 | Chiropractic, Dr. Tom Ball, Exercise, Health
I just finished a nice Sunday morning bicycle ride, and I am amazed at how many other cyclists that I saw out there riding without a helmet! I do not get it… it makes ZERO sense! When I ask people why they are not wearing a helmet I get responses like this… “I know...
Apr 30, 2019 | Chiropractic, Health
Month 2 at Performance Health Center! I am loving my work here. Treating patients every day and watching their pain levels decrease and their functional ability increase, is an amazing thing to be a part of. Spring is finally here! This month I want to talk about...
Jan 1, 2019 | Chiropractic, Exercise
That’s right. Yet another new study has come out showing the health benefits of being active, this time as it relates to longevity. The December 2018 issue of the Mayo Clinic Proceedings has a research study titled: Various Leisure-Time Physical Activities...
Dec 30, 2018 | Chiropractic, Dr. Tom Ball, Health, Newsletter, Performance Health Center
As a Doctor of Chiropractic, I see a lot of sick and injured people every day, and it is my job to help these patients get better. Yes… Chiropractic can also help with colds and flu- studies show that getting regular chiropractic adjustments helps boost the...